Disseminated intravascular coagulAtion (DIC) (BSH 2009)
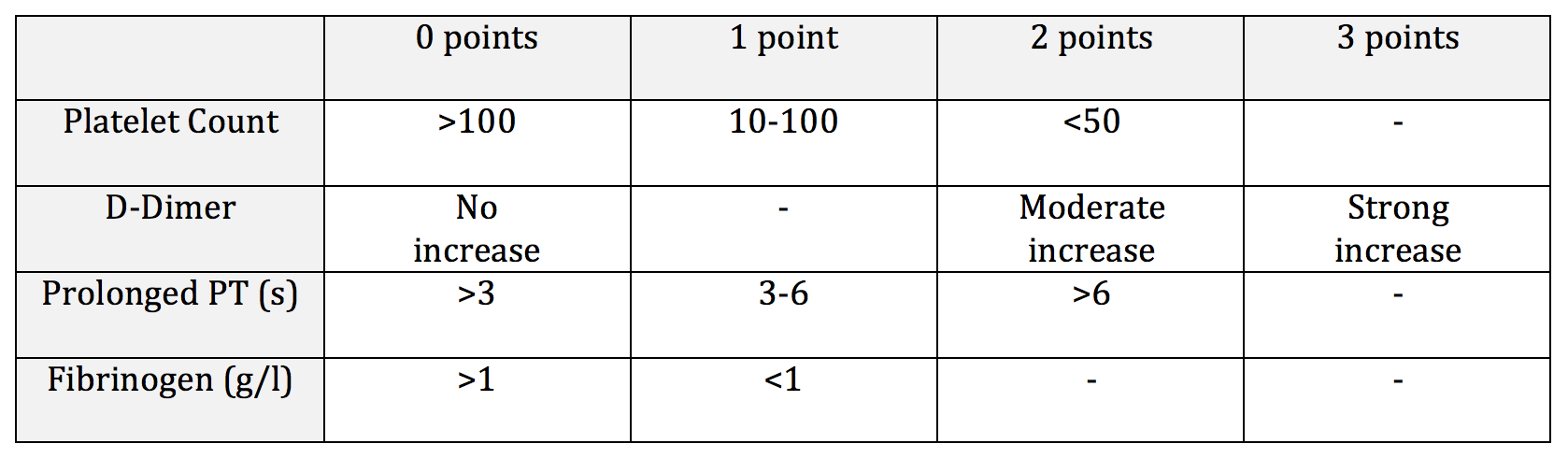
ISTH DIC Score: Score ≥5 compatible with overt DIC. Predicts mortality.
Intro
DIC is the loss of localization or compensated control of intravascular activation of coagulation
The loss of the regulated balance between procoagulant/anticoagulant and profibrinolytic/antifibrinolytic processes —> simultaneous bleeding and microvascular thrombosis at different vascular sites.
Pathophysiology
1. Excess Thrombin Generation
Excess thrombin generation results from an increased presence of tissue factor (TF), and the reason for this depends on the underlying pathology:
Infection: Increased TF expression on monocytes
Trauma: Thromboplastin-like substances released from injured tissues, e.g. brain
Obstetrics: Amniotic fluid is a rich source of TF + Phospholipid
Malignancy: TF-like proteins produced by malignant cells
Excess thrombin results in:
Clotting factor and platelet consumption --> Bleeding
Hyperfibrinolysis – Increased D-dimers and thrombin-antithrombin complexes --> bleeding
Anticoagulant consumption – reduced protein C/S, Anti-thrombin --> Thrombosis
Excess Antifibrinolysis – increased thrombin activatable fibrinolysis inhibitor (TAFI) and plasminogen activator inhibitor (PAI) --> Thrombosis
2. Mechanisms that fuel and perpetuate thrombin generation become pathogenic
3. Parallel activation of inflammatory cascade further promotes thrombin generation, e.g.
TNF activates coagulation
Thrombin activates PAR receptors and converts C5 —> C5a promoting inflammation
4. Complicated role of endothelial microvasculature in the above processes.
Clinical Features
Excess Bleeding
Depletion of coagulation factors & platelets
Abnormal platelet function in uraemia
Reduced factor production in liver impairment
Microvascular thrombosis --> Organ failure
Reduced levels of anticoagulants
Loss of thrombomodulin receptors on the damaged endothelium
Endothelial dysfunction --> reduced nitrous oxide --> uninhibited platelet activation
Treatment
1. Reverse underlying pathology
2a. If not bleeding:
No blood products unless to prepare for invasive procedure
Prophylactic LMWH should be given
(Side note: ?Recombinant activated protein C (continuous infusion for 4 days) ?fallen out of favour. 2001 trial showed increased survival in severe sepsis but with increased rate of severe bleeding. Contraindicated if platelet count <30. Stop 20 minutes prior to invasive procedures.)
2b. If bleeding:
Aim to maintain, plt >50, FGN >1.5, PT/APTT <1.5x ULN
There is no evidence that administration of FFP stimulates the ongoing activation of coagulation
Consider PCC if FFP contraindicated, but will provide only partial correction of global deficiencies.
Use cryo / FGN concentrate if FGN <1.0g/l
In general avoid tranexamic acid. Consider if hyperfibrinolytic state and severe bleeding
2c. If thrombosis predominates:
Therapeutic dose heparin infusion if significant thrombosis occurs
Differential Diagnosis for DIC
Chronic DIC
Usually thrombotic > haemorrhagic
Adenocarcinoma – thrombophlebitis migrans & recurrent VTE (Trousseau’s Syndrome)
Retained dead fetus syndrome – starts low grade, will become fulminant DIC if not evacuated
Liver disease – DIC may play a part in the coagulopathy of liver disease
Localised lesions - aneurysms, haemangiomata, empyema
Notes on Fibrinolysis
Pro-Fibrinolysis Elements
Tissue Plasminogen Activator (tPA)
Serine protease produced in endothelial cells
Under normal circumstances tPA has a half-life of 2-3 min, due to inhibition by PAI-1
In the presence of fibrin clot, tPA’s affinity for plasminogen is greatly increased
Plasminogen
Inactive zymogen that is cleaved by t-PA or u-PA —> Active Plasmin serine protease
Plasminogen deficiency very rare —> causes haemorrhagic conjunctivitis
Anti-Fibrinolysis Elements
Plasminogen Activator Inhibitor 1 (PAI-1)
A member of the serine protease inhibitor (SERPIN) family, produced in endothelial cells
t-PA:PAI-1 complexes are removed by the liver
a2-Plasmin inhibitor (a2-AP)
Major inhibitor of plasmin
Member of SERPIN family, it becomes cross-linked into fibrin clot, rendering the clot resistant to fibrinolysis.
Tissue Activatable Fibrinolytic Inhibitor (TAFI)
Removes the t-PA binding site from plasminogen, preventing its conversion to plasmin