Follicular Lymphoma (FL) (BSH 2020)
CD10+, CD19+, CD20+, BCL2+, BCL6+
CD5-, CD43-
t(14;18) IGH-BCL2 translocation
Intro
Commonest low grade lymphoma in the UK
Median age 60-65 y.o.
85% Advanced disease at presentation
Germinal centre B cell is the cell of origin (centrocyte = old morphology term)
Pathology
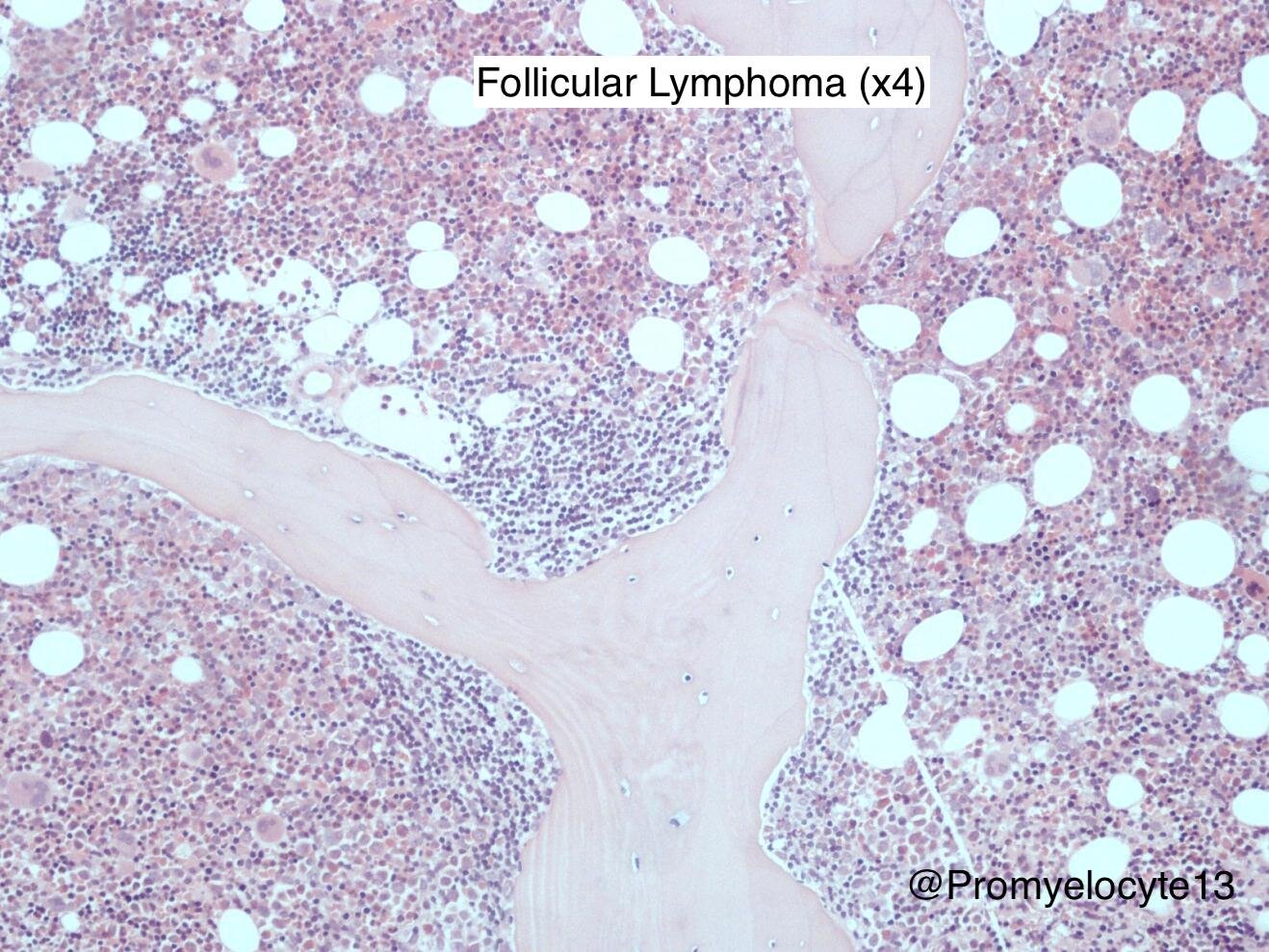
histopathology
LN excision or core biopsy required for diagnosis & grading of FL (Fine needle aspiration (FNA) is inadequate)
Can see the classic LN morphology even macroscopically
Histology Grading (WHO 2008)
1-2: 0-15 centroblasts per HPF
3: >15 centroblasts per HPF
3a: Centrocytes present
3b: Centroblasts only. Centrocytes absent. treat as if DLBCL.
Immunophenotype
CD10+ (marker of GC when present in mature lymphomas)
CD 19+, CD20+, BCL2+, BCL6+
CD43-
Cytogenetics
t(14;18) - IGH-BCL2:
Almost always present in FL.
BCL2 is an anti-apoptosis gene. Translocation next to a promoter gene —> over-expression of BCL2.
50% of healthy people have circulating t(14;18) cells, but at no increased risk of developing lymphoma. So t(14;18) is a pre-requisite of FL, but is not pathognomonic.
“FL in situ” – may occur in normal patient with circulating t(14;18) cells that happen to be passing through the germinal centre at time of biopsy. Again, no increased risk for developing lymphoma.
MLL-2 (Mixed-Lineage Leukaemia) gene:
Mutated in 90% of FL.
Gene for histone acetyl. Most frequent mutation seen in FL. Combined with t(14;18) causes FL in mice.
Others:
Great many other B cell receptor pathway mutations have been identified.
Staging
CT Neck-Pelvis
The established modality for staging FL.
PET-CT?
FL is PET avid. Upstages many people. Good way to exclude patients from radiotherapy only.
Exact role unclear and practice varies but NICE recommends PET-CT prior to stage I/II disease where radiotherapy-only treatment is planned (PET will upstage 10-60% of patients)
BM Biopsy?
Not necessarily required – Will it change the management?
(But Note: it is included in BSH list of core recommended invesitgations)
BM involvement present in approx 50% of cases at diagnosis
Prognosis
Current generalized OS is 20 years
20-30% transform to high grade lymphoma
Progression of Disease at 24 months (‘POD24’) is an important prognostic cut off, high risk group for those with a PFS shorter than 2 years after 1st line therapy.
FLIPI Score
Calculate at time of diagnosis. One point for each of:
Age >60
Raised LDH
Hb <120g/l
Stage III or IV
5 or more nodal areas involved
FLIPI score outcomes
0-1 91% 5-yr OS. 84 months median PFS
2 78% 5-yr OS. 70 months median PFS
3-5 52% 5-yr OS. 42 months median PFS
FLIPI2 Score
Created in Rituximab era. Includes age, serum B2-microglobulin, Hb, BM involvement and tumour burden.
Treatment
When to start treatment (vs watchful waiting)?
Bulk: >5cm? >7cm? >10cm? No single cut-off, patient-by-patient assessment
B Symptoms / Pruritis
Cytopenias
Organ / Bone compromise
‘Growing’ e.g. interval change on repeat CT after 3-6 months
(BNLI and GELF both have published ‘criteria to not watch & wait’ - these are listed in BSH guideline)
Watchful Waiting Vs Rituximab monotherapy
Rituximab x4 monotherapy can be offered to patients with asymptomatic, low volume disease in the UK
The W&W trial now has 12 years follow-up
Time to next treatment was 2.7 yrs for W&W versus 9.9 yrs for Ritux x4
Time to second next treatment was not reached in any arm, no significant differences observed
What?
The only good quality evidence demonstrating an increase in OS is for the addition of Rituximab to Chemotherapy.
Most other data refer to PFS, e.g. no change in OS with R-maintenance.
Therefore, in young patients the question is not which treatment is best, but rather which order is best
Stage 1 (or 2 in a single nodal group)
50% cure rate with full surgical excision or radiotherapy (in UK)
Radiotherapy - typically IFRT 24 Gray in 12 daily fractions (in UK). FORT Trial is assessing RT dosing.
Stage 2a treated with ISRT —> 10-yr disease-free survival 50% & only 1% relapse within the radiotherapy field, i.e. curative if truly localised disease.
Stage 2 in different nodal group
Unusual scenario, patient-by-patient assessment
1st Line in advanced disease
Rituximab-Chemo
Obinutuzumab-Chemo (Gallium trial)
(Not FCR – toxic, too high a TRM rate)
(R2 – Rituximab + Lenalidomide – used in USA)
Choice of 1st line chemo (with ritux)
No conclusive evidence to favour on regimen over another.
CHOP – Previous standard of care. TRM 1% in Gallium trial. ?Waste of anthracycline upfront
Benda – Probably better PFS & better tolerated during treatment (fewer neutropenic infections than CHOP). But longer term severe infections in 6 months post treatment —> TRM 5% in Gallium (PCP pneumonia)
CVP – lower CR rate and shorter PFS
Choice of 1st line Anti-CD20
Rituximab – standard of care, plenty of historical data
Obinutuzumab – Gallium trial. Small but statistically significant increase in PFS (NNT = 25 to delay 2nd line treatment). No difference in OS. More toxic, especially in combo with bendamustine.
R-Maintenance post 1st line
Every two months for two years. Prolongs PFS.
Based on PRIMA trial, which used R-CHOP —> Not strictly approved for post R-Benda but we do in East of England.
Controversial – medicalizes patients for two years and increases risk of severe infection. Does not alter OS.
Autograft?
Consider for fit patients if relapse within 2 years of 1st line therapy, i.e. POD24
May provide 10-15 year remission
2nd Line if remission >2 years, or not fit for autograft
One of the above that had not been used 1st line
Remember should aim to re-biopsy at relapse
R-maintenance can be used again after completion of re-induction chemotherapy
3rd Line
Epcoritamab (CD3xCD20) - monotherapy after 2+ lines of therapy (NICE 2026) (Lancet Haem 2024)
Consider clinical trial
GemCis / DHAP / Bendamustine
Not Idelasilib (PI3K delta/gamma inhibitor) – too toxic, CMV/PCP deaths.
car-t?
Autologous T-cells modified in vitro and then re-infused so as to target tumour cells
There are different generations of CAR-T in development as the technology progresses, but broadly the CAR-T cells have a new cell surface receptor (the Chimeric Antigen Receptor) that targets the tumour cells (e.g. CD19 for DLBCL) and new internal signalling domains that promote cytotoxic activity when the surface receptor is activated.
Not yet available for follicular lymphoma outside of clinical trials in the UK (as of Dec 2023)
See this 2020 BMT review paper for a succinct overview of CAR-T (but in high grade lymphoma)
A few trial notes
Watch & Wait 12 year outcomes (2022)
Phase 3, 460 patients with asymptomatic, low tumour burden follicular lymphoma
3 arms: W&W vs Ritux x4 (RI) vs RI followed by Ritux maintenance (RM)
Median TTNT 2.7 yrs W&W, 9.9 yrs RI, not reached for RM
At 10 yrs, 28% W&W, 49% RI and 64% RM had not started a new treatment
Median TT2NT not reached in any arm
No significant difference in OS at 10 years
RELEVANCE Trial 2018
Phase 3, 1000 patients
Rituximab-Lenalidomide (R2) for 18 cycles vs R-Chemo for advanced, previously untreated FL
Both arms received R-maintenance.
Negative trial. Designed as superiority trial and did not meet this.
Non-significant higher CR and PFS for R-Chemo
GALLIUM Study 2017
Obinutuzumab-Chemo vs Rituximab-Chemo for previously untreated FL
Improves PFS. No OS difference
PRIMA Trial 2011
Randomised, open label, 1200 patients
2 years R-maintenance vs observation only post local first line standard of care chemo
10 year update released – 10-yr PFS 51% with, 35% without. No OS difference at 10 years
StiL Study 2013
R-Benda vs R-CHOP for previously untreated FL
PFS better with R-Benda. No OS difference.